If we cannot solve vaccine equity globally, we cannot escape variants locally: Bhramar Mukherjee
Living through the pandemic has taught us some valuable lessons about how to live through uncertainty and prepare for it, the professor of biostatistics, University of Michigan School of Public Health writes on the biggest lessons and what she thinks 2022 will bring
 With waning immunity and breakthroughs, a large number of infections can happen quickly and even a small fraction of that needing hospital admissions is going to crumble the fragile health care system
With waning immunity and breakthroughs, a large number of infections can happen quickly and even a small fraction of that needing hospital admissions is going to crumble the fragile health care system
Image: Danish Siddiqui/ Reuters
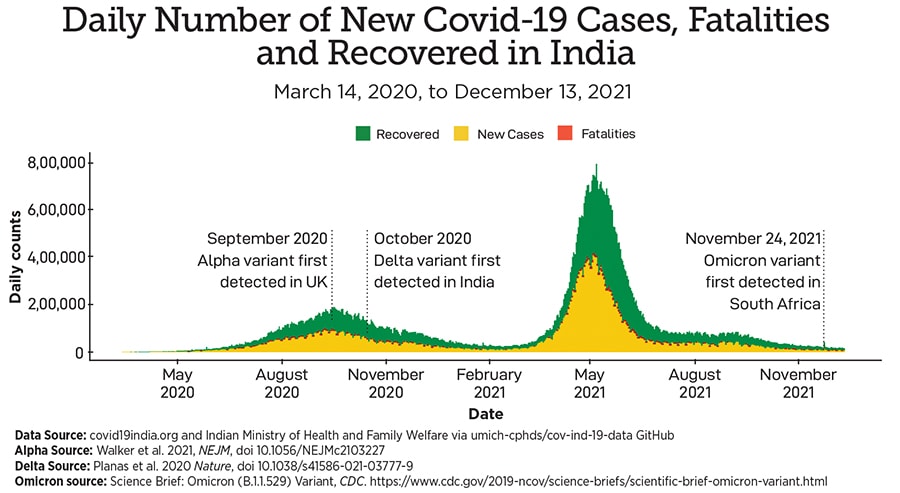
 In the last two years I, like many of my friends, have lived, breathed, and sighed on the epidemiology of Sars-Cov-2. When our team started modeling the trajectory of this insidious virus in India in March 2020, none of us expected the pandemic to last this long. We ended 2020 on an optimistic note, with multiple vaccines showing promising efficacy results in clinical trials and receiving emergency use authorisations. The rollout of the vaccines brought tears of joy to millions of eyes as we welcomed 2021. Those moments will always represent the triumph of science and humanity to me. However, after this uber-uncertain vaccine-versus-variant roller-coaster of 2021, first Delta and then Omicron, we have learned some key lessons as we embark on the journey in 2022. Here are my top five lessons from 2021, followed by a summary of what I think 2022 may bring for
In the last two years I, like many of my friends, have lived, breathed, and sighed on the epidemiology of Sars-Cov-2. When our team started modeling the trajectory of this insidious virus in India in March 2020, none of us expected the pandemic to last this long. We ended 2020 on an optimistic note, with multiple vaccines showing promising efficacy results in clinical trials and receiving emergency use authorisations. The rollout of the vaccines brought tears of joy to millions of eyes as we welcomed 2021. Those moments will always represent the triumph of science and humanity to me. However, after this uber-uncertain vaccine-versus-variant roller-coaster of 2021, first Delta and then Omicron, we have learned some key lessons as we embark on the journey in 2022. Here are my top five lessons from 2021, followed by a summary of what I think 2022 may bring for
(1) We need global collaboration to end this pandemic; it is a synchronised relay race of the whole world together, if there is something like relay marathon. No country can possibly get ahead of the other, there is no quick solitary win here. If we cannot solve the issue of vaccine equity globally, we cannot escape the variants locally. A colleague of mine aptly said if we replace the “I” in illness by “we”, it becomes wellness. In this time of contagion, our own potential outcome does affect the outcome of others. Due to this spillover effect, we must make individual sacrifices for the collective good.
(2) The need for robust and transparent public health data systems and large cohorts with integrated data. Many of the key papers on Covid have come out of the UK, Israel and Denmark due to their national health/insurance systems database or population-based cohorts. Integrating testing, vaccination, sequencing databases with clinical data were key to identifying new variants and characterising their immune escape, transmissibility, and lethality properties. These multi-platform, cross-talking databases also gave us real-time data on vaccines and their effectiveness.
In the early days of Covid, they primed us about who is at the highest risk of hospitalisation due to Covid. When I started working on the India data, the data-paucity was eye opening. It is nearly impossible to find national level age-sex disaggregated counts on Covid deaths. Many deaths get unregistered, undercounted. After two years of Covid I am yet to see the daily hospitalisation data across India. Some data sources exist on governmental websites, but it takes incredible amount of effort to web-scrape and collate them in a usable format for running models.
(This story appears in the 30 November, -0001 issue of Forbes India. To visit our Archives, click here.)