India's Covid-19 vaccines can definitely be cheaper. Will its makers agree?
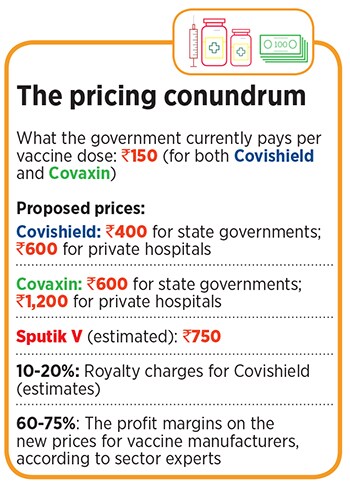
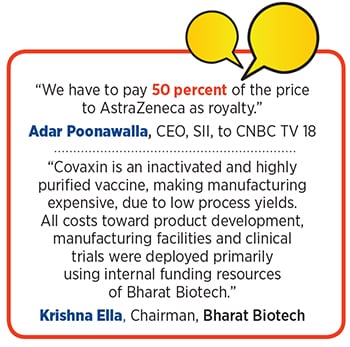
As vaccine manufacturers announce higher prices for states and the private sector, we find out that it's actually possible to make vaccines affordable. A look at the factors that influence prices, and who stands to benefit

A rice mill worker receives a dose of Covishield, a coronavirus disease (Covid-19) vaccine manufactured by Serum Institute of India, during a Covid-19 vaccination drive at Bavla village on the outskirts of Ahmedabad, India, April 13, 2021. Credit: Amit Dave / Reuters
It’s been a gloomy few weeks in India.
Across cities and towns, a raging second wave of the Covid-19 pandemic has wreaked havoc and brought its crippled health care sector to its knees. Many states have resorted to lockdowns to restrict movement, as beds, ventilators, and even oxygen supply run short. In April alone, over 30,000 people have died, as daily cases surged from less than 15,000 on March 1, to 3.5 lakh on April 26. That number is expected to swell in the coming weeks, even as questions have been raised about its veracity, with inadequate testing, and underreporting of death in some states.
Amidst all this, the Narendra Modi government is desperately trying to ramp up vaccinations, to bring some reprieve to the situation. Perhaps taking a cue from Israel’s successful vaccination policy, and vaccine hesitancy among many Indians, the government now reckons that vaccinating a wider group as quickly as possible is key to ending the pandemic, even though it had initially envisaged an entirely different vaccination programme. The initial plan was to vaccinate 300 million people, including health care and frontline workers by July, before vaccinating everyone else.
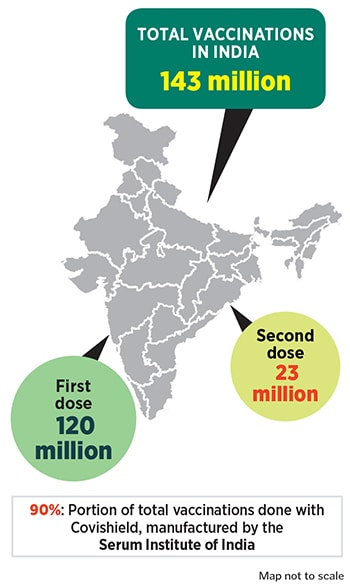
From May 1, some 60 percent of the population will be eligible for vaccinations, even as concerns have been raised about the availability of vaccines. India is undertaking the world’s largest vaccination programme, and only last week extended it to those between the age of 18 and 45, who account for more than 40 percent of the population.