Some philanthropists are supporting mental health causes. More should follow the lead
India is at the starting point of understanding mental health and making services accessible to people. While the government has a huge role to play, we need more philanthropists in this space, and they need to do better
 From L to R: Rohini Nilekani, Kris Gopalakrishnan, Harsh Mariwala, Kiran Mazumdar-Shaw
From L to R: Rohini Nilekani, Kris Gopalakrishnan, Harsh Mariwala, Kiran Mazumdar-Shaw
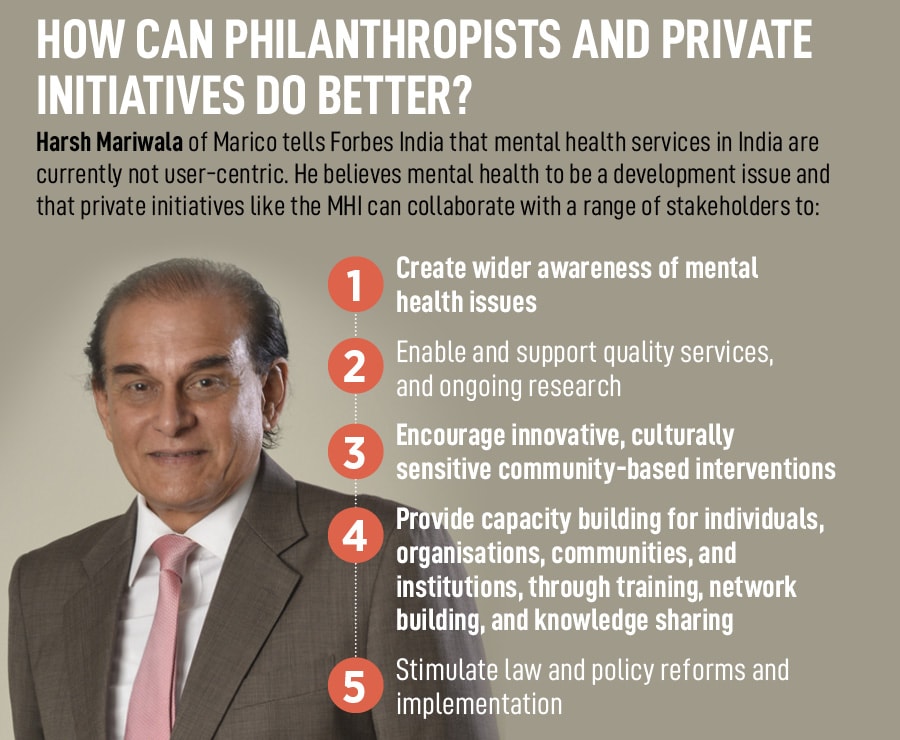
Harsh Mariwala, founder of FMCG company Marico, raises an important point. Why is data around suicide, a health indicator, collected as part of crime data? This has real implications, he says. “For example, if we go to a locality and ask for people who have attempted suicide. Any person whom we identify has a risk of being questioned by the police as suicides are still [a] medico-legal issue,” the founder of Mariwala Health Initiative (MHI) that focuses specifically on mental health issues, tells Forbes India over email. “It is also possible that sharing a past experience can be traumatic for the person.”
MHI seeds the Alliance for Suicide Prevention in India that collaborates with organisations, activists, funders, researchers and policymakers to prevent suicides at individual and community levels. As per the latest available statistics from the National Crime Records Bureau (NCRB), 164,033 people died by suicide in 2021, a 7.2 percent increase from 2020. Collecting data around suicide requires understanding of the context, ensuring affected people have access to helplines or other support, and respecting their right to privacy, Mariwala explains. “There is a need to have a public health approach which looks at data carefully, leverages community resources, has inter-sectoral collaboration and uses data to design prevention solutions,” he says.
There is a lot to unpack here. About how supporting people with mental health issues needs to leverage community help, how it takes different stakeholders to do their part and work together, how they all need to work with sensitivity and empathy. And treating mental health as health is the starting point of all this.
Mariwala is among a handful of businesspersons who has been dedicatedly working to improve people’s access to mental health services through MHI. A few other philanthropists and organisations who have been supporting mental health causes at scale include Wipro Chairman Azim Premji, Biocon CMD Kiran Mazumdar-Shaw, Tata Trusts and Aditya Birla Education Trust.